MELANOMA: SKIN CANCER THAT KILLS
MELANOMA: SKIN CANCER THAT KILLS
By Carol Duff MSN RN STAFF WRITER
University of Toledo
School of Medicine/College of Nursing
Normally the skin produces a protein called melanin made by melanocytes, which are located in the bottom layer of skin. Melanin absorbs ultraviolet (UV) radiation in response to exposure to the sun. The melanin tries to protect the skin by absorbing the UV radiation and produces a tan when the skin is exposed to sunlight.
People with dark brown or black skin have the same number of melanin producing cells, but produce more melanin and are less likely to have skin that is damaged by UV radiation. Non-cancerous growth of melanocytes produces moles and freckles. Cancerous growth of melanocytes produces melanoma. Malignant melanoma is responsible for over 1% of all cancer deaths.
 Melanoma often occurs in adults who are in the prime of their lives. Some traits and factors that can be associated with the incidence of melanoma are:
Melanoma often occurs in adults who are in the prime of their lives. Some traits and factors that can be associated with the incidence of melanoma are:
-
Multiple moles
-
Non-typical moles
-
Family tendency to have atypical moles
-
Disorders of natural repair of the skin
-
Too much exposure to the sun
-
Freckling
-
Painful or blistering sunburn
-
Burns easily
-
Unable to tan
-
Light hair and/or blue eyes
Melanoma starts on the surface of the skin, but if given time to grow may extend down into the skin and reach the blood and lymphatic systems and spread to other parts of the body and cause a life-threatening illness.
Melanoma
Skin cancer is the most common of all cancers and is also the easiest to cure if diagnosed and treated early. Self-examination is an important way to catch melanomas at their earliest stage of development.
- Everyone. including children. who can be taught at an early age.
- Your doctor or dermatologist at your medical examinations.When Should Skin Self-Examinations be Done?
- Often and examinations of the skin should become a habit. Find a few moments at least every three months.
- The Self-examination should start with the head and end with the feet.
- Self-examination should include the scalp, face, neck, beneath facial hair and trunk.
- On the upper part of the body, self-examination should include the armpits, hands including palms, finger webs, and nail beds.
- A mirror should be used to examine the back and skin between the buttocks.
- On the legs, which also should include toe webs, toe nail beds and soles of the feet.
- If you are comfortable with having someone assist with areas it is diffiicult for you to see, please enlist their help in this process.
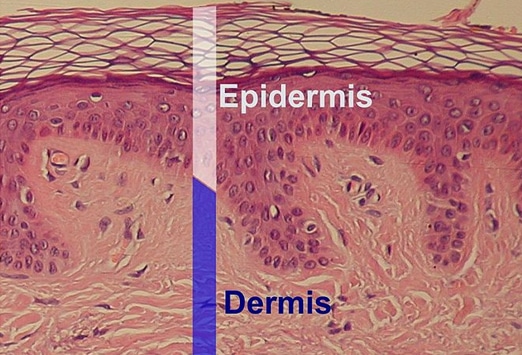
Genes control cell growth and melanoma is thought to be uncontrolled growth of the melanocytic stem cells with the eventual invasion into surrounding tissue. If the melanoma is only in the outer layer of skin (epidermis) this is called melanoma in situ and the cure is always excision of the questionable area because there is no potential spread to other parts of the body.
If the cancerous cells have penetrated deeper through the skin layers this is called invasive melanoma. Once the melanoma cells have reached the lower layers of skin (dermis) there is a chance that the cancerous cells can spread by accessing the lymphatic system to the local lymph nodes or through the blood stream where is can reach organs such as the brain and lungs.
The chance of a secondary spread or further spread of the cancer (metastasis) depends on how deep the melanocytic cells have penetrated into the skin. Early detection of melanoma will stop this spread of cells and is of utmost importance.
WHAT ARE SOME OF THE RISKING FACTORS?
-
Sun exposure, especially during childhood
-
Fair skin that burns easily
-
Blistering sunburn, especially when young
-
Previous melanoma
-
Previous non-melanoma skin cancer (basal cell carcinoma or squamous cell carcinoma.
-
Family history of melanoma, especially if two or more members are affected
-
Large numbers of moles (especially if there are more than 100)
-
Abnormal moles which are a larger size and/or have irregular borders
WHERE DO YOU LOOK TO FIND MELANOMAS?
One half of the melanomas appear on normal looking skin or from a mole or freckle which starts to grow larger and changes in its appearance. Other lesions (abnormal areas of the skin) which can be the start of a melanoma are:
-
Brown birthmark
-
Strange looking mole
-
Normal looking mole
-
Can appear anywhere on the body, not just areas that received sun exposure. For men the back is the most common site and for women the most frequent site is the leg.
-
Melanoma usually start on the skin, but can grow on mucous membranes such as the lips and genitals. Sometimes a melanoma may grow on the eye, brain, mouth, or vagina.
What Does a Melanoma Look Like?
-
The first sign may be a changed or new freckle or mole.
-
Unusual shape.
-
May be seen when they are small at an early stage, but can grow much larger.
-
May start as a flat area and then become raised.
-
May have several colors including tan, dark brown, black, blue, red and sometimes light grey. There are melanomas that are the color of normal skin or are white or scarred in appearance.
-
May or may not be itchy or tender. More advanced areas will bleed easily and then crust over.
-
Although not all melanomas show these characteristic,s there is a seven point checklist (Glascow) with major and minor features and also the ABCDE’s of melanoma.
-
Change in size
-
Irregular shape
-
Irregular color
-
Diameter less than 7 mm (about one fourth of an inch)
-
Inflammation
-
Oozing
-
Change in sensation
ABCDE’s of melanoma
A. Asymmetry
B. Border irregularity
C. Color variation
D. Diameter over 6 mm (size of a pencil eraser)
E. Evolving (enlarging, changing)
Asymmetry; one half unlike the other half.
Border;
irregular, scalloped or poorly defined border.
Color; varied from one area to another; shades of tan and brown, black; sometimes white, red or blue.
Diameter; while melanomas are usually greater than 6mm (the size of a pencil eraser) when diagnosed, they can be smaller.
As many as five percent of melanomas disappear from sight after a period. It is at this time that they may have already spread into the body before a doctor can look at them. The disappearance of the loss of visible melanoma cells on the skin results from the body’s attempt to kill the melanoma cell with its own immune cells and antibodies.
As the body’s immune system attempts to kill the melanoma cells, the area of skin that surrounds the melanoma may also be killed and this produces the halo effect of a white ring around the melanoma.
If there is a diagnosis of melanoma, the doctor will examine the whole body to check if cancer cells have spread to other areas of the body such as nearby lymph glands. A careful exam of the skin will determine whether there are more suspicious areas of the skin.
Melanomas are surgically removed and the extent of the surgery depends on the thickness of the melanoma and where it is located. For thicker melanomas the lymph glands near the melanoma area will be tested or removed.
What is Mole Mapping?
Mole mapping is a surveillance program for those who are at high risk of malignant melanoma. This may include a clinical skin examination and dermoscopy (close examination of the skin using skin surface microscopy to elevate pigmented skin lesions) to closely evaluate a suspected skin area.
Mole mapping may involve marking spots on a drawing of the body, print photographs, or digital images of the whole body’s skin surface. This mapping may be reviewed at a latter date to see if there are new skin lesions or whether existing lesions have grown, changed color, or shape.
What is Digital Mole Mapping?
Sophisticated digital mole mapping may include:
- Risk evaluation (medical and family history, skin typing, sun exposure)
- Patient education about sun protection, moles, and melanoma
- Skin examination by a health professional (usually a doctor or specially trained nurse)
- High quality digital images
- Poses of the whole body with areas of lesions of concern localized
- Close-up images of the lesions of concern
- Dermascopic images of lesions of concern
-
Evaluation of the images by an expert in skin cancer
-
A report to the patient and or referring health practitioner including suspected diagnoses and recommendations for treatment of lesions of concern
-
Follow-up mole mapping in three to six months for lesions of concern that are not ready for excision
-
Follow-up mole mapping of all imaged lesions a one or two year intervals
-
A secure database and transfer system to store images and reports
-
Copies of images for the patient or doctor to aid self skin examination
Who is Suitable for mole mapping? Mole mapping is useful for those who have:
-
Lots of moles (more than 50 to 100)
-
Moles that are large, have an unusual color or shape
-
Moles on the back which are hard to keep track of
-
Strong family history of melanoma
-
Moles and fair skin which has been severely sunburned
-
Any concern about individual moles or freckles due to appearance or recent change
Advantages of mole mapping:
-
To diagnose melanoma at the earliest stage
-
Identify new lesions or changes in pre-existing lesions
-
The previous record can be used to determine whether a lesions if new or has changed
-
If the doctor decides that the lesions should be removed, this should be done at the earliest possible stage which will reduce the risk of melanoma and minimize surgery
-
If the lesion has changed or is new, but not necessarily at the threshold for removal, it can be re-imaged and watched carefully.
-
Lesions which are not melanomas may not need to be removed which will reduce the potential cost and complications of surgery.
-
Digital mole mapping may be achieved near where you live
-
Earlier evaluation by an expert
-
Reassurance for the patient
Risks of mole mapping:
-
Mole mapping is a new procedure and is considered experimental by many dermatologists
-
There may be a melanoma in a site that has not been imaged (scalp, genitals)
-
A harmless lesion may be misdiagnosed as melanoma
-
Early melanoma may look like a normal mole and might really be positive for cancer
-
A melanoma may grow rapidly and may reach a dangerous size before the next scheduled visit for mole mapping
-
The procedure may be embarrassing
References
American Academy of Dermatology (2009). Malignant Melanoma. Retrieved April 1, 2009 from http://www.aad.org/public/publications/pamphlets/sun_malignant.html
Ignatavicius, D.& Workman, M. (2006). Medical-surgical nursing:Critical thinking for collaborative care (5th edition). St. Louis, MO: Elsevier Saunders.
New Zealand Dermatological Society Incorporated (2009). Retrieved March 11, 2009 from http://dermnetnz.org/lesions/melanoma.html
Silberman, Allan. Malignant Melanoma. Retrieved March 31, 2009 from http://www.cancernews.com/articles/melanomas.htm
Weber, Paul (1997). Melanoma, Malignant Melanoma. Retrieved April 1, 2009 from http://www.skincancerinfo.com/melanoma/melanoma.html
Carol Duff is a Nurse Educator specializing in veterans medical problems and staff writer for VT.

Carol graduated from Riverside White Cross School of Nursing in Columbus, Ohio and received her diploma as a registered nurse. She attended Bowling Green State University where she received a Bachelor of Arts Degree in History and Literature. She attended the University of Toledo, College of Nursing, and received a Master’s of Nursing Science Degree as an Educator.
She has traveled extensively, is a photographer, and writes on medical issues. Carol has three children RJ, Katherine, and Stephen – one daughter-in-law; Katie – two granddaughters; Isabella Marianna and Zoe Olivia – and one grandson, Alexander Paul. She also shares her life with her husband Gordon Duff, many cats, and two rescues.
ATTENTION READERS
We See The World From All Sides and Want YOU To Be Fully InformedIn fact, intentional disinformation is a disgraceful scourge in media today. So to assuage any possible errant incorrect information posted herein, we strongly encourage you to seek corroboration from other non-VT sources before forming an educated opinion.
About VT - Policies & Disclosures - Comment Policy