Each year, approximately 12,000 women in the U.S. get cervical cancer. As the second most common cause of cancer deaths in women, cervical cancer has an impact on females around the world.
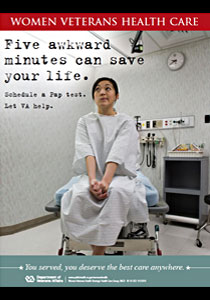
Dr. Laurie Zephyrin, the national director of Reproductive Health at the Department of Veteran Affairs, says making screenings part of a woman’s regular physical can save lives.
For her, the goal to increased and early detection is simple and clear.
“It’s about ensuring access to high quality care and educating women on how to take care of themselves.”
Screening
The first step of care is informing women of the critical test for cervical cancer: the Pap test. The test reveals abnormalities in cells in the cervix. It can detect cancer early, when treatment is most effective.
U.S. Preventive Services Task Force guidelines recommend a Pap test starting at age 21; from ages 21 to 65, the test should be at least every 3 years. For patients over 65 with normal Pap test results for several years, the doctor may say it’s OK to stop getting regular screenings. However, patients should speak with their health care provider — the frequency of screenings may vary based on past Pap tests, past surgeries, or age.
Dr. Zephyrin cautions that an abnormal Pap test does not mean a patient has cervical cancer.
“Depending on the test result, sometimes it requires something as simple as repeating the Pap test or taking a closer look at the cervix with an electronic microscope called a colposcopy. With a closer view of the cervix, many abnormalities seen can be biopsied and sent to the lab for a more in-depth evaluation.”
Another test that can be included with the Pap test is one that screens for the human papillomavirus, or HPV. On its own it is not a routine screening test. But infection with certain types of high risk HPV, a sexually transmitted infection, can be associated with cervical cancer.
Many sexually active people will contract HPV at some point in their lives but few will get cancer. HPV infection may be cleared over time. Condoms offer some protection against HPV infection, and one can also decrease the risk of infection by limiting the number of sexual partners.
Persistence of the HPV infection and progression to cancer can be influenced by poor nutrition, a suppressed immune function (from autoimmune diseases such as HIV/AIDS), and cigarette smoking.
Female Veterans younger than 26 can receive a vaccination called Garadasil or Cervarix that prevents high-risk strains of HPV. Despite vaccination they should still have regular Pap tests.
Taking Care of Women Veterans
Cervical cancer screenings are one of the VA’s quality measures and it’s a quality measure VA takes seriously. In both 2008 and 2009, 92 percent of women ages 21 to 64 who were enrolled in a health plan had received at least one Pap test in the past 3 years.
According to the 2010 VA Hospital Report Card, “Overall, provision of gender-specific care to women, e.g., screening for breast and cervical cancer, substantially exceeded that in other settings including commercial managed care systems, Medicare and Medicaid.”
With more women Veterans receiving VA health care each year, Dr. Zephyrin reports VA is employing a comprehensive approach in caring for women Veterans.
“We definitely need to continue to ensure that our women Veterans are provided routine gynecological care and that women are receiving the best care in a timely fashion. It’s very important that women Veterans know that they can come to us to get their care.”
– From the VA
ATTENTION READERS
We See The World From All Sides and Want YOU To Be Fully InformedIn fact, intentional disinformation is a disgraceful scourge in media today. So to assuage any possible errant incorrect information posted herein, we strongly encourage you to seek corroboration from other non-VT sources before forming an educated opinion.
About VT - Policies & Disclosures - Comment Policy