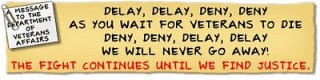
Drugs have one job and that is to get people to feel better. Antibiotics stop infections so that the body can take over and heal the wound. When it comes to PTSD, medications cover up the pain but too many times they cause more problems. When drugs are all that is used to fight PTSD, it isn’t giving troops a fair fighting chance to heal.
Army Trauma Unit’s Woes Detailed
By JAMES DAO
Published: January 26, 2011The Army units created to provide special care for wounded soldiers after the Walter Reed Army Medical Center scandal continue to struggle with short staffing, inadequate training and an overabundance of prescription medications, a report by the Army inspector general’s office said.
Clinician’s Guide to Medications for PTSD
What is the evidence base for the specific groups of medications used for PTSD treatment?
Selective Serotonin Reuptake Inhibitors (SSRI’s). These medications are the only FDA approved medications for PTSD . SSRIs primarily affect the neurotransmitter serotonin which is important in regulating mood, anxiety, appetite, and sleep and other bodily functions. This class of medication has the strongest empirical evidence with well designed randomized controlled trials (RCT’s) and is the preferred initial class of medications used in PTSD treatment (1, 2). Exceptions may occur for patients based upon their individual histories of side effects, response, and comorbidities. An example of an exception would be a PTSD patient with comorbid Bipolar Disorder. In this patient, there is a risk of precipitating a manic episode with the SSRI’s. Each patient varies in their response and ability to tolerate a specific medication and dosage, so medications must be tailored to individual needs. Research has suggested that maximum benefit from SSRI treatment depends upon adequate dosages and duration of treatment. Treatment adherence is key to successful pharmacotherapy treatment for PTSD. Examples of the SSRI’s and some typical dosage ranges are listed below:sertraline (Zoloft) 50 mg to 200 mg daily
Injury Law
The FDA posted a warning on its website at the beginning of February 2005 and required Zoloft’s manufacturer, Pfizer, to include a warning on the label that Zoloft was among the drugs that “increased the risk of suicidal thinking and behavior in short-term studies of adolescents and children.”
Later information indicated that Zoloft might pose a similar threat to adults and the FDA issued a Public Health Advisory warning on July 1, 2005 warning that studies had raised the possibility of increased risk of suicidal behavior in adults treated with antidepressants.
citalopram (Celexa) 20 mg to 60 mg daily
FDA Issues Proposed Revisions to Celexa Blackbox Warning
In 2009, based on new evidence of suicide and suicidal or dangerous behavior in adults taking antidepressants, the FDA proposed revising the blackbox warning to include the increased risk in patients up through the age of 24. The proposed Celexa warning outlines the age groups that are most at risk for suicide, suicidal thoughts and suicidal behavior according to short-term studies. Those groups most at risk include children, adolescents and young adults ages 24 and younger. The risk decreases beyond age 24. The proposed revision recommends close monitoring while patients are taking Celexa and for those in high risks groups, that the benefit from the drug be closely weighed against the possible risks.
In other words any young soldier under 24 should not be given this drug.
paroxetine (Paxil) 20 to 60 mg dailyThe Bottom-Line
Paxil
It is now generally recognized that SSRIs, including Paxil, can cause a condition called akathisia (severe inner restlessness) that is associated with suicidal tendencies. In Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (“DSM IV TR”) under Differential Diagnosis it states: “Serotonin-specific reuptake inhibitor antidepressant medications may produce akathisia . . .” “Akathisia may be associated with dysphoria (restlessness, depression & anxiety), irritability, aggression, or suicide attempts.”In October 2003, the FDA notified healthcare professionals of reports of the occurrence of suicidal tendencies (both suicidal ideation and suicide attempts) in clinical trials for various antidepressant drugs in pediatric patients with major depressive disorder.
Then, in March 2004, the FDA issued a Public Health Advisory that provides further cautions to physicians, their patients, and families and caregivers of patients about the need to closely monitor both adults and children with depression, especially at the beginning of treatment, or when the doses are changed with either an increase or decrease in amount.
Shortly after the release of the Public Health Advisory, the FDA and GlaxoSmithKline notified healthcare professionals of revisions to the warnings and precautions of Paxil labeling to alert healthcare professionals that patients with major depressive disorder may experience worsening of their depression and/or the emergence of suicidal ideation and behavior (suicidal tendencies), whether or not they are taking antidepressant medications.
fluoxetine (Prozac) 20 mg to 60 mg daily
Note: Only Sertraline and Paroxetine have been approved for PTSD treatment by the FDA. All other medications described in this guide are being used “off label” and may have empirical support but have not been through the FDA approval process for PTSDOther Newer Antidepressants for PTSD. Antidepressants that work through other neurotransmitter combinations or through different mechanisms for altering serotonin neurotransmission are also helpful in PTSD. Venlafaxine acts primarily as a serotonin reuptake inhibitor at lower dosages and as a combined serotonin and norepinephrine reuptake inhibitor at higher dosages. It appears to be a first-line treatment for PTSD based upon large multi-site RCTs (6). There have been smaller RCT’s with mirtazapine as well as open trials (7). Mirtazapine may be particularly helpful for treatment of insomnia in PTSD. Trazodone is also commonly used for insomnia in PTSD even though there is little empirical evidence available for its use. Nefazodone is still available in a generic form but carries a black box warning regarding liver failure, so liver function tests need to be monitored and precautions taken as recommended in the medication’s prescribing information (8, 9). Examples of the newer antidepressants for PTSD and some typical dosage ranges are listed below:
ulmirtazapine (Remeron) 7.5 mg to 45 mg daily
venlafaxine (Effexor) 75 mg to 300 mg daily
nefazodone (Serzone) 200 mg to 600 mg daily
All of the antidepressants described above are also effective in treating co-morbid Major Depressive Disorder (MDD) which often accompanies PTSD. While bupropion is useful in treating comorbid MDD, it has not been shown effective for PTSD in controlled trials (10). A recent trial showed superior outcomes on MDD when mirtazapine was combined initially with antidepressants vs. patients being randomized to monotherapy with fluoxetine (11). This raises important questions regarding costs, side effects, and patient preferences which merit further study.Mood Stabilizers for PTSD. Despite some promising open label studies, recent RCT’s have been negative for this group of medications in treating PTSD (12). They could be helpful in the treatment of co-morbid Bipolar Disorder and PTSD, however. For patients who have Bipolar Disorder and PTSD, these medications are useful due to the potential for antidepressants to precipitate a manic episode. Most require some regular lab work to monitor side effects. Lamotrigine does not require lab work but must be titrated slowly according to package insert directions to avoid a potentially serious rash. Examples are given below:
Carbamazepine (Tegretol): Requires monitoring of white blood cell counts due to risk of agranulocytosis. Will self-induce its own metabolism and increase the metabolism of other medications including oral contraceptives.
Divalproex (Depakote): Requires monitoring of liver function tests due to risk of hepatotoxicity and platelet levels due to risk of thrombocytopenia. Target dosage is 10 times the patient’s weight in pounds.
Lamotrigine (Lamictal): Requires slow titration according to the package insert due to risk of serious rash.
Atypical Antipsychotics for PTSD.While originally developed for patients with a psychotic disorder, this class of medications is being applied to patients with many other psychiatric disorders including PTSD. They act primarily on the dopaminergic and serotonergic systems and are being used in PTSD for improving hyperarousal and re-experiencing symptoms. The evidence is mixed on their use as adjunctive therapy in PTSD for patients who have residual symptoms following the use of first line agents such as SSRI’s and venlafaxine (13).There is currently one positive trial for risperidone as monotherapy. This trial studied women with PTSD related to sexual assault and domestic abuse. There are three positive trials and two negative trials of risperidone as adjunctive therapy. Many of the studies using risperidone as adjunctive therapy included veterans with combat trauma. For olanzapine, there is one negative trial as monotherapy and 1 positive trial as adjunctive therapy. There are currently no published randomized placebo controlled trials for any of the other atypical antipsychotic agents.
These medications must be used with caution and require monitoring of blood glucose levels and cholesterol levels as they may cause elevation. There is also a small risk of developing extrapyramidal side effects and tardive dyskinesia and more rare side effects such as neuroleptic malignant syndrome. These medications are also effective for comorbid psychotic and mood disorders for which they are approved. Dosages vary widely, so please refer to package insert for dosing ranges.
Olanzapine (Zyprexa)
Risperidone (Risperdal)
Other Medications for PTSD. There are a number of other medications that can be helpful for specific PTSD symptoms or that have been used as second line agents including the following:Prazosin (Minipress)
Tricyclic Antidepressants (such as Imipramine)
Monoamine Oxidase Inhibitors (MAOI’s) (such as Phenelzine)
Prazosin has been found to be effective in RCTs in decreasing nightmares in PTSD. It blocks the noradrenergic stimulation of the alpha 1 receptor. It has not been found to be effective for PTSD symptoms other than nightmares at this time (14). The tricyclic antidepressants and MAOI’s act on a number of neurotransmitters. While there are RCT’s supporting their use, these medications are not used as first line agents due to their safety and side effect profiles (15, 16). The tricyclics have quinidine like effects on the heart and can cause ventricular arrhythmias especially in overdose. The MAOI’s can cause potentially fatal reactions due to hypertensive crisis when taken with other medications or certain foods rich in tyramine. MAOI’s can also provoke the potentially fatal serotonin syndrome when used concurrently with SSRI’s.Buspirone and beta blockers are sometimes used adjunctively in treatment of hyperarousal symptoms, though there is little empirical evidence in support of this. Buspirone acts on serotonin and might reduce anxiety in PTSD without sedation or addiction. There are some case reports supporting its use. Beta blockers block the effects of adrenalin (epinephrine) on organs such as the heart, sweat glands, and muscles. There is interest in using beta blockers to prevent PTSD, though the evidence at this time does not support this. Beta blockers reduce the peripheral manifestations of hyperarousal and may reduce aggression as well. They may be used for comorbid conditions such as performance anxiety in the context of social phobia for example.
Benzodiazepines and PTSD. Benzodiazepines act directly on the GABA system which produces a calming effect on the nervous system. This is the only potentially addictive group of medications discussed. Studies have not shown them to be useful in PTSD treatment as they do not work on the core PTSD symptoms (17, 18). There are several other concerns with the benzodiazepines including potential disinhibition, difficulty integrating the traumatic experience, preventing optimal arousal in prolonged exposure therapy, and addiction. Because of their potential for addiction and disinhibition, they must be used with great caution in PTSD. Examples are listed below:
Lorazepam (Ativan)
Clonazepam (Klonopin)
Alprazolam (Xanax)
Just giving medication and no therapy does not work. Drugs can make PTSD worse, just cover-up the symptoms instead of healing the cause of the symptoms. Yet this has been the practice. Many older veterans in the VA system are finding their appointments with mental health therapists are being cut back because of the newer veterans flooding the system. The point of medication is supposed was supposed to be to make patients better, not numb them. When your body is feeling pain, doctors find out what the cause of it is and do something about it. They will give pain killers to get you out of pain for now but that is not their only answer to treating you. The same path to wellness should be part of mental healthcare. Healing means healing and not just stopping the feelings.
The report was a result of growing complaints from the soldiers in those units about the quality of care they were receiving as well as from their commanders about the discipline problems posed by some soldiers.
The New York Times described complaints from soldiers about overmedication, a lack of therapists and long waits for medical discharges in an article last year about the Warrior Transition Unit at Fort Carson, Colo.
A final word regarding medications and treatment for PTSD:
A more comprehensive discussion of pharmacotherapy can be found at www.healthquality.va.gov in the VA/DoD PTSD Clinical Practice Guidelines. Based upon current knowledge, most prescribing clinicians view pharmacotherapy as an important adjunct to the evidenced based psychotherapies for PTSD. While there are few direct comparisons of pharmacotherapy and psychotherapy, the greatest benefits of treatment appear to come from evidenced based therapies such as CPT, PE, and patients need to be informed of the risks and benefits of the differing treatment options. When using a combined approach of medication and therapy, it is important to keep several practices in mind. If treatment is being provided by a therapist and a prescriber, it is important for the clinicians to discuss treatment response and to coordinate efforts. It is important for the prescribing clinician to have an ongoing dialogue with the patient about their medications and side effects. It is important for the patient to take an active role in his or her treatment rather than feeling they are a passive recipient of medications to alleviate their symptoms. There is emerging evidence that when given a choice, most patients will select psychotherapy treatment for their PTSD symptoms rather than medications.Patients with anxiety disorders including PTSD may be very aware of their somatic reactions, and it is important to start low and go slow often on dosage adjustments to improve patient adherence. Be sure to ask female patients of childbearing age about contraception when prescribing medication. Be sure to ask all patients about substance abuse as well. Once mediations are started, it is crucial that the provider remember to discontinue medications which are not proving efficacious and to simplify the number and types of medications used whenever possible.
The transition units have long been criticized by some commanders as dumping grounds for soldiers not fit to deploy. That concern is raised in the report, which notes that just 10 percent of the transition unit soldiers had been physically wounded in combat, while the rest had mental health problems or noncombat-related injuries or illnesses.
Many soldiers in the units are taking medications for post-traumatic stress disorder that make them forgetful, irritable or disoriented — thereby causing tensions with their platoon sergeants.
The report said that many of the platoon sergeants and leaders themselves felt they were not qualified to handle soldiers on medications or with mental health problems, and they wanted better training.
Each medication comes with warnings but no one seems to be paying attention to them anymore than they paid attention to the fact that most of these medications include instructions that a doctor monitor the patients. In other words, sending them back into combat on these medications offering warnings against driving or operating machinery is not a good idea considering they are doing a lot more than just driving.
PTSD is a wound but it is a wound causing emotional pain. They need to be able to feel something so they can heal it.
This is an update to this post. It is not just about meds for PTSD but for pain as well. This Lt. General came out and talked about his own battle.
Lt. Gen. David Fridovich puts troops first ahead of pride
When you think that Lt. Gen. David Fridovich could have kept this part of his life private but decided to put the troops ahead of his privacy, that is one remarkable man! He is not a low profile serviceman who would make a good local story but someone with a lot of power to make things happen. Just coming out and talking about this will do wonders for others making them think that if he’s talking about it, they can too. If he healed, they can too. If he is not ashamed, they don’t have to be either.3-star opens up about battle with addiction
Army Lt. Gen. David Fridovich says that, for years, he has regularly consumed narcotics and painkillers to deal with chronic pain — and now he’s sharing his story
By Gregg Zoroya – USA Today
Posted : Wednesday Jan 26, 2011 21:38:59 EST
TAMPA, Fla. — Standing before a packed hall of 700 military doctors and medics here, the deputy commander of the nation’s elite special operations forces warned about an epidemic of chronic pain sweeping through the U.S. military after a decade of continuous war.Be careful about handing out narcotic pain relievers, Lt. Gen. David Fridovich told the audience last month. “What we don’t want is that next generation of veterans coming out with some bad habits.”
What Fridovich didn’t say was that he was talking as much about himself as anyone.
For nearly five years, the Green Beret general quietly has been hooked on narcotics he has taken for chronic pain — a reflection of an addiction problem that is spreading across the military. Hospitalizations and diagnoses for substance abuse doubled among members of U.S. forces in recent years. This week, nurses and case managers at Army wounded care units reported that one in three of their patients are addicted or dependent on drugs.
“This is huge for Fridovich to be willing to talk about this as a three-star general,” says Gen. Peter Chiarelli, Army vice chief of staff. “We’re finally coming clean and admitting at all levels this is an issue.”
Fridovich says narcotics altered his personality, darkened his mood and management style, and strained his 35-year marriage.
When Fridovich finally went through treatment and detoxification to reduce his drug reliance in 2008 — he still relies on weaker doses of narcotics to combat pain — his wife, Kathy, hid or destroyed more potent pain pills so he could not use them.
read more here
Lt. Gen. David Fridovich puts troops first ahead of pride
ATTENTION READERS
We See The World From All Sides and Want YOU To Be Fully InformedIn fact, intentional disinformation is a disgraceful scourge in media today. So to assuage any possible errant incorrect information posted herein, we strongly encourage you to seek corroboration from other non-VT sources before forming an educated opinion.
About VT - Policies & Disclosures - Comment Policy